uti infections are one of the most common reasons patients receive prescription antibiotics[1-2]

With a prevalence of 11%, UTIs are amongst the most common community and healthcare acquired infections. Between 50-60% of adult women will experience at least one UTI in their lifetime, with recurrence observed in approximately 27% of patients within 6 months[3].
While uncomplicated UTIs of the lower urinary tract cause discomfort, they are not life-threatening. However, they are a significant cause of morbidity amongst the elderly (aged 65+) where diagnosis and antibiotic treatment is often difficult[4]. Additionally, complicated UTIs (~2% of annual hospitalizations[5]) can be unresponsive to antibiotics, leading to more serious complications such as kidney damage or urosepsis, associated with a mortality rate of ~10%[6].
Standard UTI treatment is often empirical, based solely on symptom assessment. Standard urine culture (SUC), the current gold standard for bacterial identification and AST, is time-consuming (48-72h) and requires sample transport to a central laboratory with skilled personnel[7]. Thus, it is not performed routinely. Common quick dipstick tests are based on secondary effects of bacteria and exhibit low sensitivity (<50%). Misdiagnosis is thus unfortunately common, resulting in 40-60% of unnecessary antibiotic treatments[8]. This overconsumption of antibiotics contributes significantly to the global antimicrobial resistance crisis[9].
Unjustified use of antibiotics in primary UTI care is associated with many problems:
References
[1] M.Gharbi et al. Antibiotic management of urinary tract infection in elderly patients in primary care and its association with bloodstream infections and all cause mortality: population based cohort study. BMJ 2019; 364 doi: https://doi.org/10.1136/bmj.l525 (Published 27 February 2019)Cite this as: BMJ 2019;364:l525
[2] M. Pujades-Rodriguez et al. Lower Urinary Tract Infections: Management, Outcomes and Risk Factors for Antibiotic Re-prescription in Primary Care / EClinicalMedicine 14 (2019) 23 31 https://doi.org/10.1016/j.eclinm.2019.07.012
[3] M. Medina and E. Castillo-Pino, ‘An introduction to the epidemiology and burden of urinary tract infections’, Ther Adv Urol, vol. 11, p. 1756287219832172, 2019, doi: 10.1177/1756287219832172.
[4] L. Rodriguez-Mañas, ‘Urinary tract infections in the elderly: a review of disease characteristics and current treatment options’, Drugs Context, vol. 9, pp. 2020-4–13, 2020, doi: 10.7573/dic.2020-4-13.
[5] M. D. Zilberberg, B. H. Nathanson, K. Sulham, and A. F. Shorr, ‘Descriptive Epidemiology and Outcomes of Hospitalizations With Complicated Urinary Tract Infections in the United States, 2018’, Open Forum Infect Dis, vol. 9, no. 1, p. ofab591, Jan. 2022, doi: 10.1093/ofid/ofab591.
[6] Z. Tandogdu et al., ‘Urosepsis 30-day mortality, morbidity, and their risk factors: SERPENS study, a prospective, observational multi-center study’, World J Urol, vol. 42, no. 1, p. 314, May 2024, doi: 10.1007/s00345-024-04979-2.
[7] D. Fraile Navarro, F. Sullivan, A. Azcoaga-Lorenzo, and V. Hernandez Santiago, ‘Point-of-care tests for urinary tract infections: protocol for a systematic review and meta-analysis of diagnostic test accuracy’, BMJ Open, vol. 10, no. 6, p. e033424, Jun. 2020, doi: 10.1136/bmjopen-2019-033424.
[8] C. Llor et al., ‘Diagnosing probable urinary tract infections in nursing home residents without indwelling catheters: A narrative review’, Clin Microbiol Infect, pp. S1198-743X(24)00419–1, Aug. 2024, doi: 10.1016/j.cmi.2024.08.020.
[9] P. C. Chardavoyne and K. E. Kasmire, ‘Appropriateness of Antibiotic Prescriptions for Urinary Tract Infections’, West J Emerg Med, vol. 21, no. 3, pp. 633–639, Apr. 2020, doi: 10.5811/westjem.2020.1.45944.
antimicrobial resistance and reducing over-consumption

The emergence of antibiotic-resistant pathogens has been deemed one of the top global health threats of our modern society. According to the WHO “antimicrobial resistance undermines modern medicine and puts millions of lives at risk”[10].
With a lack of pipeline drugs, we are already facing challenges in treating common infections – with serious consequences for patient health outcomes and global economies.
Thus, there is an urgent unmet need for novel, rapid and reliable UTI diagnostics to detect a bacterial infection, so that the most appropriate treatment can be prescribed immediately. Increased consumption of antibiotics is directly related to the increase in antibiotic resistance.
References
[10] ‘Report signals increasing resistance to antibiotics in bacterial infections in humans and need for better data’. Accessed: Sep. 02, 2024. [Online]. Available: https://www.who.int/news/item/09-12-2022-report-signals-increasing-resistance-to-antibiotics-in-bacterial-infections-in-humans-and-need-for-better-data
uti testing at centralized laboratories

Today urine samples are often sent to centralized labs for culturing which:

Takes 1-3 days to receive complete results from tests

Requires specialized staff at every stage of testing
Requires laboratory equipment with large capital expenditure
decentralized uti testing

Decentralizing UTI testing saves time to result, and with Utilizer’s novel technology the results can be obtained during the same day.
Utilizer’s new innovative technology allows the UTI testing to be performed at the point-of-care reliably. Benefits of moving UTI testing to the point-of-care is to shorten the time to result, support physicians in their treatment decisions, avoid unnecessary consumption of antibiotics and diminishing discomfort for the patient.
Benefits of Utilizer’s novel technology to be used in decentralized settings:
Decentralized settings can be anywhere a health care professional can perform a test.
Typical places include:
General Practioner’s Offices / Community Clinics
Health Care Centers / Primary Care
Acute Care / Urgent Care
Elderly Care

Web Doctors
Today health care is under immense pressure and all paths to reduce costs are searched for, therefore leaning the patient flows and treating the patients where they first get in contact with health care has proven to be efficient. Utilizer’s technology has the potential of enabling reliable UTI testing to be done in point-of-care, near the patient.
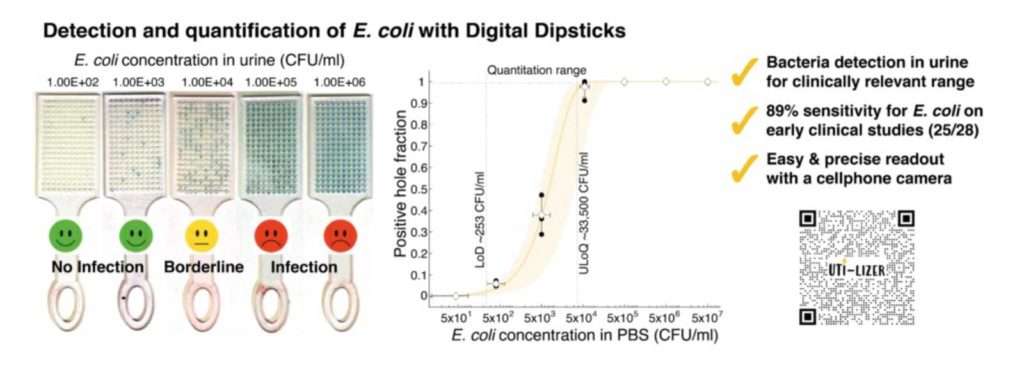
Utilizer’s technology:
Scientific Publications
Emre Iseri, Sara Nilsson, Alex van Belkum, Wouter van der Wijngaart and Volkan Özenci (2024). Performance of an innovative culture-based digital dipstick for detection of bacteriuria. Microbiology Spectrum, 12(1), e03613-23. (Link)
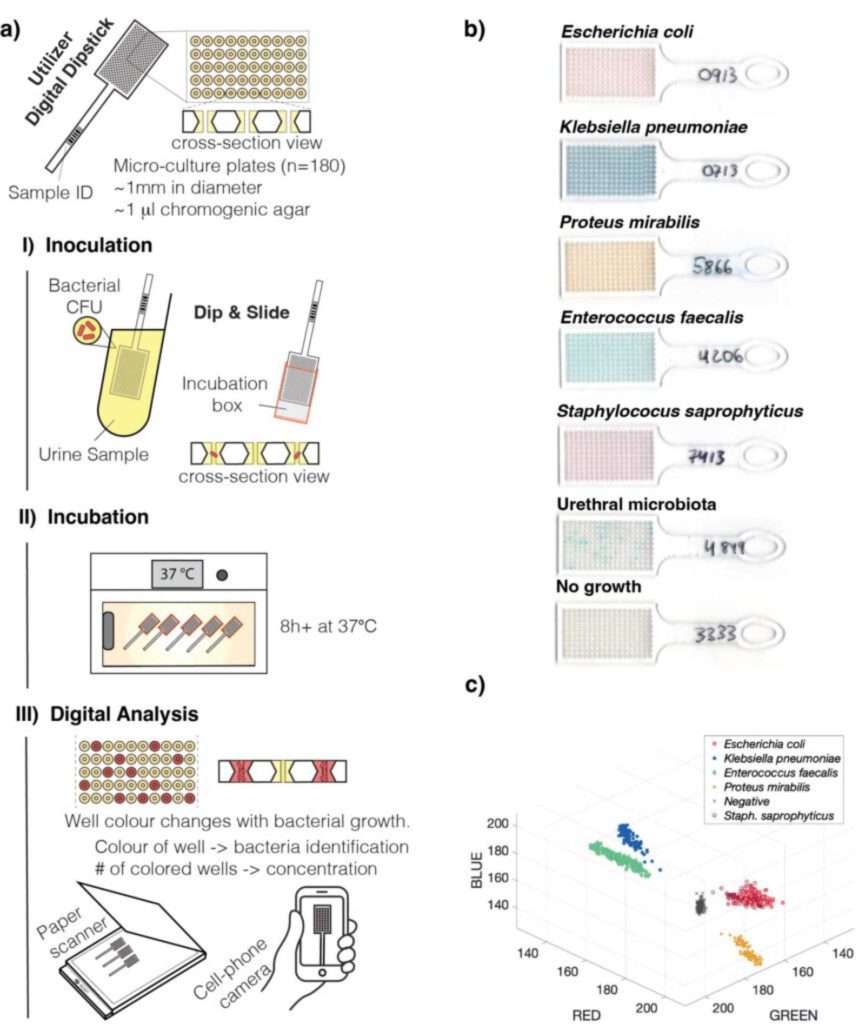
Emre Iseri, Michael Biggel, Herman Goossens, Pieter Moons, and Wouter van der Wijngaart. “Digital dipstick: miniaturized bacteria detection and digital quantification for the point-of-care.” Lab on a Chip 20, no. 23 (2020): 4349-4356. (Link)
Scientific Conferences
- Emre Iseri, Sara Nilsson, Alex van Belkum, Wouter van der Wijngaart and Volkan Özenci. “Digital Point-of-care culture for urinary tract infections.” 33rd European Congress of Clinical Microbiology & Infectious Diseases (ECCMID). Copenhagen, Denmark 2023.
- Emre Iseri, Angelos Valandis Miliadis, and Wouter van der Wijngaart. “A Digital Dipstick for Multiplexed Bacteria Detection.” Miniaturized Systems for Chemistry and Life Sciences (MicroTAS). Palm Springs, USA (virtual) 2021.
- Emre Iseri and Wouter van der Wijngaart. “Digital Dipstick: Point-of-care Diagnostic Test for Urinary Tract Infectiousssay.” DIATECH 2020, European Conference on Novel Technologies for In Vitro Diagnostics. Leuven, Belgium 2020.
- Emre Iseri, Seref Akay, and Wouter van der Wijngaart. “Detection of E. coli in a digital assay.” IEEE Micro Electro Mechanical Systems (MEMS). Belfast, UK, 2018.
